bezpestkowe

Harmful stereotypes still persist in our society - gender is often defined by the condition of our bodies. Those of us who feel feminine are well aware that the absence of a uterus does not take anything away from us, does not make us 'incomplete'. Our condition therefore proves that gender identity has no right to be defined by what our bodies have and don't have.
MRKH syndrome does not subjugate Bezpestkowe’s femininity - it is about time for this to ring loud and clear, especially since as Bezpestkowe we are often excluded from the so-called 'women's circles', where bonds are often established on the foundation of shared experiences of menstruation and motherhood. Knowing what it feels like to be excluded from communities, we do our best to avoid creating a similar atmosphere within our own.
Just as among the general population, there are non-binary, transgender and non-heteronormative people among us. For this perhaps small but no less significant group of Bezpestkowe, the preconception that we are all heterosexual women leads to an even stronger sense of exclusion. Out of respect for our diversity and the desire to create a community where everyone can be themselves regardless of gender identity and psychosexual orientation*, we use the words 'patient' and 'person' interchangeably and refrain from specifying the gender of Bezpestkowe’s potential partners.
There are also intersex people among us. What is intersex? Inter-sex is an umbrella term for people who are born with a body that does not fit into social and/or medical definitions of typical female or male bodies. People with MRKH can (but don’t have to) identify under the intersex umbrella.

MRKH syndrome is a genetically determined aplasia (organ failure) or hypoplasia (significant underdevelopment) of the uterus and vagina in a person with a female phenotype (ed. note: phenotype most simply explained means the appearance of a person) with karyotype 46.XX. It belongs to the group of rare diseases because, according to statistics, it affects about 1 in 4000 to 1 in 10 000 live born female newborns (most often it is said that it is about 1 in 4500 live born female newborns). In Poland there are approx. 4400 people with MRKH, and about 40 Bezpestkowe are born each year.
MRKH syndrome looks different in each person. It ranges from a complete absence of the uterus, to residual non-functioning uterine horns or residual uterine horns with a residual cavity with endometrium. Similarly, in the case of the vagina, it may be completely absent, present in a vestigial form or in the form of a recess, which in some individuals is large enough to become a fully functional vagina without medical intervention when intercourse is attempted.
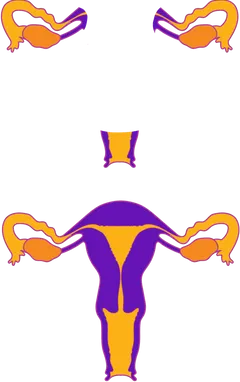
MRKH syndrome is complex - in medicine, anything called a syndrome is made up of many components. Defects of the uterus and vagina can therefore be accompanied by defects in other organs. The two systems most commonly affected are the urinary system and the skeletal system; in some cases there are also defects of the heart and great vessels, and some patients have hearing loss.
There are therefore two types of MRKH syndrome: the first is diagnosed when the defect is limited to the reproductive system, i.e. the uterus and vagina, and the second when other defects coexist, such as congenital absence of a kidney and/or spinal defects.
Although Bezpestkowe do not menstruate, this does not equate to the absence of a menstrual cycle. People with MRKH syndrome have functioning ovaries that secrete hormones and produce ova, so Bezpestkowe ovulate and, hormonally speaking, go through all the stages of the cycle. The only difference is that there is no bleeding, although in the presence of a vestigial endometrium "micro-menstruation" may occur. Bezpestkowe will also go through menopause and may experience the many discomforts associated with it.
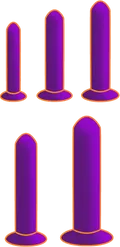
Having MRKH does not equal being unable to have sex. Each person defines sex in their own way, and penetration is not necessary. However, if you choose to have penetrative sex, there are three ways to create a vagina. Remember to check with your health care provider before doing this. Whichever option you choose, successful and satisfying sex despite MRKH is possible. The quality of sex does not depend on whether your vagina is 4 or 7 centimetres long, but on who you choose to have sex with.




MRKH puberty (up to the point of diagnosis) follows the same patterns as a cis women’s puberty, so Bezpestkowe usually take on female gender roles (because of their physical appearance, not MRKH syndrome).
The role of a therapist is to support people with MRKH in engaging in sexual contacts, or to jointly identify the reason why they do not. Talking through the mental blocks and finding solutions to them helps achieve sexual satisfaction.
Each person, regardless of having or not having a seed, is built differently - our bodies, their appearance and functionality are different. If you are concerned that your sexual partner(s) will recognise that your vagina has been produced, we assure you that there is no need to worry - from a layperson's point of view, we are unable to recognise whether we are having sexual contact with a person who was born with a vagina or a person who has a neo-vagina. Another consequence associated with MRKH syndrome is the inability to get pregnant and give birth. Usually when MRKH is identified, this information is more difficult for parents/carers of Bezpestkowe to accept. Of course, having MRKH does not preclude you from becoming a parent (that is of course if you want to become one at all). There are different ways to do this:


The first option is uterine transplantation, which is still considered an experimental treatment and for anatomical reasons cannot be performed on all patients with MRKH syndrome. Currently, there are more than ten children born to patients with MRKH in the world. To date, the best-known precedents are those of 2014 and 2017, when, in Sweden and Brazil respectively, patients with MRKH gave birth - in the first case from a uterus transplanted from a living donor, in the second from a deceased donor. The uterus is not a vital organ and is only transplanted for one pregnancy (it is removed after birth). Although the operation is very complicated and burdensome for both the donor and the recipient, it is possible.
A second option is surrogacy, which involves ectopic fertilisation with transfer of the embryo to a surrogate mother. In this way, a patient with MRKH syndrome can be a genetic parent, since from an ovarian point of view Bezpestkowe are fertile.
The third (and currently the only legally available in Poland) option is adoption, but in order to initiate the adoption procedure, one must be married for at least four years.
It is worth noting that there are individuals who fulfil the need for parenthood in other ways, e.g. by bonding with a person who has a child/children, by becoming involved as a carer, a close family friend, etc.